Research
Central consequences of peripheral nerve repair
Peripheral nerve injury is the most common nerve trauma, the consequences of which significantly burden Health Care Systems in civilian and military populations. Peripheral nerve injuries that occur clinically as either complete transections or ablations of a segment of a major nerve often exhibit very poor, if any, behavioral recovery with contemporary clinical practice. After these nerve injuries, motor and sensory function distal to the injury is completely lost due to interrupted axonal continuity, and the distal portions of axons always and irreversibly undergo degeneration. Protracted functional recovery can occur slowly through regenerating axon outgrowths from surviving proximal axons that often very inaccurately (non-specifically) reinnervate target tissues that may atrophy before reinnervation occurs.
In collaboration with colleagues at the University of Texas at Austin, we have been working on a novel repair strategy that produces dramatically better outcomes than what is achieved with standard clinical practice. This axonal repair technique consists of a series of pharmaceutical agents including the membrane fusogen polyethylene glycol (PEG), in conjunction with microsuturing of the proximal and distal nerve segments. Importantly, this repair technique dramatically improves the rate and extent of behavioral recovery and prevents much axonal degeneration and muscle atrophy; PEG-fusion rapidly re-establishes and maintains continuity for many axons, and distal target NMJs remain functionally innervated.
My lab is particularly interested in the central consequences of the PEG-fusion repair. Importantly, there is no expectation of PEG-fusion to reconnect specific individual proximal axons with their distal partner. In the PEG-fused animal, projections from motoneurons to their original target muscles can be 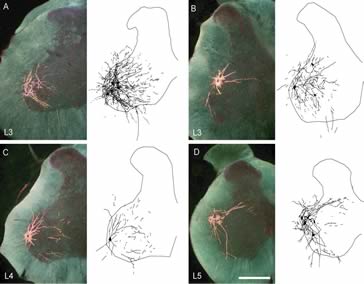 restored, but novel projections are introduced as a consequence of mis-pairings of axons at the repair site. Despite these mispairings, PEG-fused motoneurons with inappropriate spinal to peripheral connections are somehow producing dramatically better behavioral recovery than is ever produced by conventional nerve repair or regeneration. We are examining the effects of PEG repair on the morphology of spinal motoneurons, looking for clues that will reveal the basis of the remarkable plasticity that must be occurring.
restored, but novel projections are introduced as a consequence of mis-pairings of axons at the repair site. Despite these mispairings, PEG-fused motoneurons with inappropriate spinal to peripheral connections are somehow producing dramatically better behavioral recovery than is ever produced by conventional nerve repair or regeneration. We are examining the effects of PEG repair on the morphology of spinal motoneurons, looking for clues that will reveal the basis of the remarkable plasticity that must be occurring.
